PGT-A: the current look at preimplantation genetic testing
PGT-A (preimplantation genetic testing for aneuploidies) is a very frequently used test all over the world. Most IVF programs perform PGT-A. Many of them only biopsy the embryos and ship the biopsy to another lab for analysis. And other centers (like ours), which have the needed technology, analyze it within the same clinic, with the advantages that this represents.
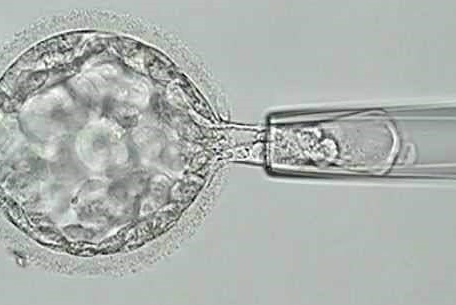
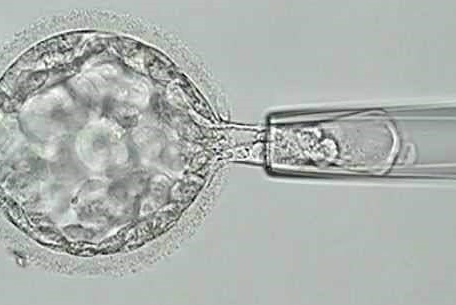
PGT-A has had different nomenclatures and acronyms in the past: PGD (preimplantation genetic diagnosis) and PGS (preimplantation genetic screening) are some of them. But in addition to changing its name, it changed many other important aspects over the years. Perhaps, two of the most relevant are: a) biopsy of the embryos is not performed any more on day 3, but now it is performed at the blastocyst stage (day 5 or 6); b) the technology do the analysis has changed many times, passing through FISH, PCR, arrays and NGS, among others.

History of PGT-A and its changes
The first change was a substantial milestone given that the results when doing the biopsy on day 3 were not good and, after the publication of several studies with negative results, its use did not grow. The fact of being able to reach the blastocyst stage, made the technique have a boom again. This made it possible to biopsy the embryos at that stage where there are more cells and where the potential impact should be less.
The second change came from the hand of technology. These changes usually bring advantages but may be accompanied by some disadvantages. Doing NGS today was beneficial in some ways, but it increased the number of so-called “mosaic” embryos. These embryos, which have some normal cells and some abnormal cells, are often not transferred to the uterus. The problem with these cases is that, it is known, some of them could give rise to healthy live births.
Is it worth doing PGT-A?
This is a difficult question to answer since it has advantages and disadvantages (like almost all technologies). However, if they are not properly evaluated, some errors could be made in the interpretation of the possible scenarios. It is well known that PGT-A does not increase the cumulative live birth rates. This is obvious since it is a diagnostic technique that would serve to make a better embryo selection, but it should not improve the implantation potential of any of the embryos.
What advantages could it have?
A good embryo selection would save money on unnecessary transfers of abnormal embryos. In addition, it would reduce the miscarriage rate and frequency of negative results (with all the negative feelings that these entails). And it would also allow to shorten the time to pregnancy (especially if there is availability to do a selection among several embryos and, therefore, the possibility of choosing the “correct” one would allow shortening the time until success is achieved).
Finally, it would reduce the chances of having a child with chromosomal abnormalities (such as Down syndrome, Edwards syndrome or Pateau syndrome). It is worth adding one more case where it could be beneficial: there are egg donor programs (like ours) that “guarantee” the transfer of at least one chromosomally normal embryo; in these cases, it would increase the pregnancy rates and the live birth rates. This is widely used by our patients, and highly recommended in surrogacy programs.
And what are the disadvantages?
There are at least two possible problems that would justify that in many published studies, the cumulative pregnancy rates with PGT-A are somewhat lower than those without PGT-A. On the one hand, there could be a potential damage to the embryo that could reduce the implantation potential. On the other hand, there are some false positives. Either the embryos that were diagnosed as abnormal (some could be normal) or the mosaics that are not transferred, could eventually give rise to a few more healthy live births.
And then, do we have to do PGT-A or not?
Unfortunately there is no single clear answer to this. It is important to know the advantages and disadvantages of this technique and to discuss its usefulness in each particular case with your own doctor. In many cases, the advantages of doing PGT-A outweigh the disadvantages. Some examples may be in cases of repeated implantation failures, treatments in some women over 40 years old, egg donation in some programs and surrogacy, among others. And in other cases, no.
And the future of the PGT-A?
Fortunately, new non-invasive techniques are being developed and could solve some of the questions we have now. But they are not yet routinely available, so we will have to continue waiting for these techniques, and continue discussing the role of PGT-A today and in each patient.