What is PGT-A and Why is it Increasingly Performed in IVF Cycles?
Preimplantation genetic testing for aneuploidies, commonly referred to as PGT-A, has become increasingly popular in the past decade. It is a technique used during in vitro fertilization (IVF) cycles to analyze the chromosome constitution of an embryo by performing a biopsy usually on days 5-6.

Evidence Supporting PGT-A: What Outcomes Are Strongest and Weakest?
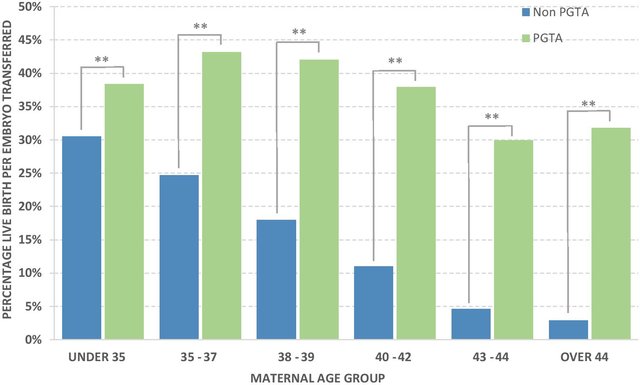
The evidence supporting PGT-A varies for different outcomes. The strongest evidence supports a higher live birth rate per embryo transfer when PGT-A is performed compared to not doing it. However, evidence for other outcomes such as a reduction in miscarriage rate, abnormal pregnancies, and time to pregnancy is weaker or scarce. Additionally, there is no evidence of benefit on cumulative live birth rate, and there is some evidence that it may actually decrease.
Concerns Regarding PGT-A: Accuracy, Viability, and Discarding Normal Embryos
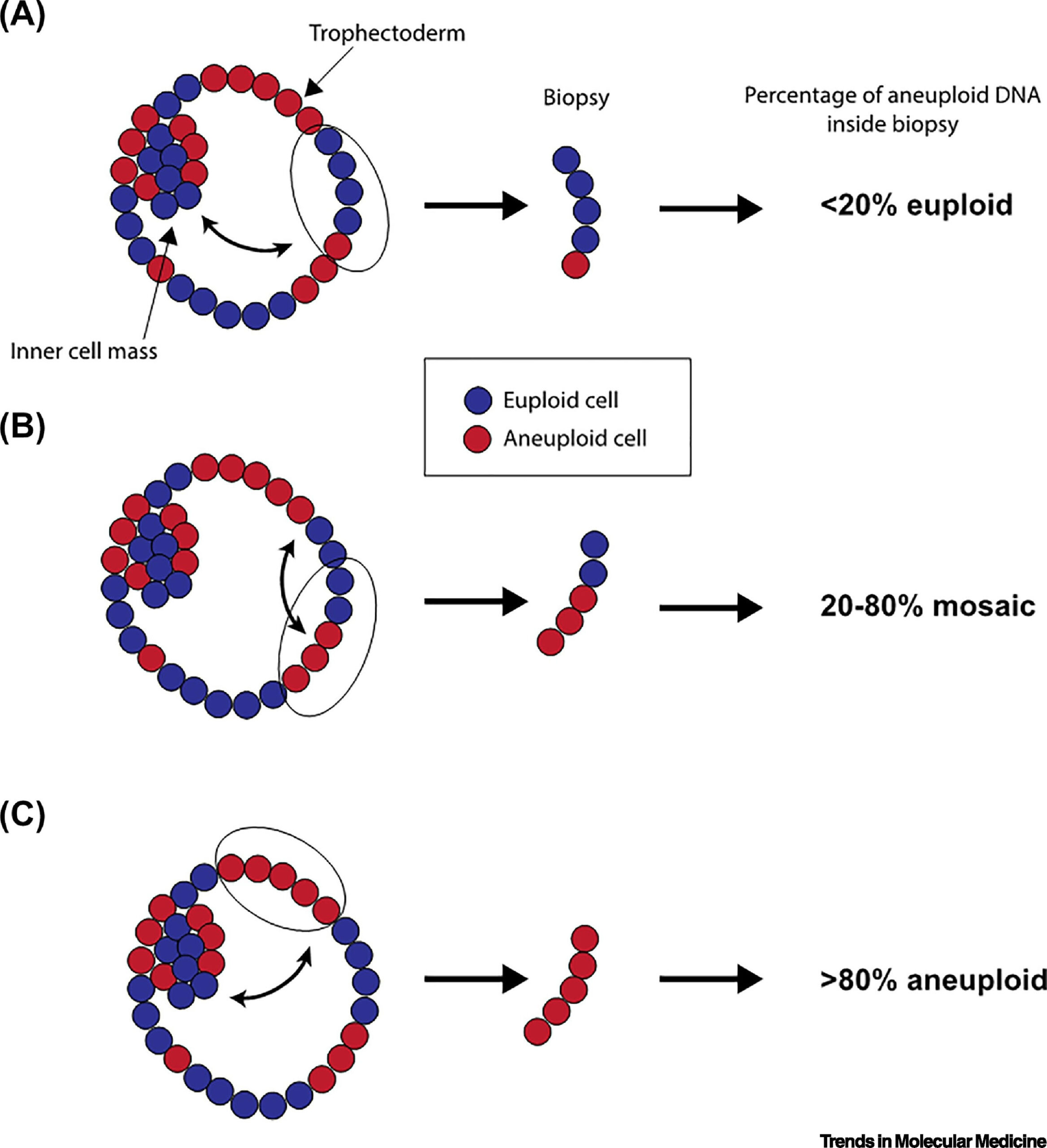
One of the main concerns regarding PGT-A is the accuracy of the technique and how it is reported, as well as the potential harm to the embryo. Although the damage rate post-biopsy is low, there is a potential reduction in the inner cell mass, which is the predecessor of the fetus. There is also a concern about discarding normal embryos due to a high false positive rate, especially related to mosaicism.
Mosaicism and PGT-A: Overdiagnosis and the Impact on Cumulative Live Birth Rate
Mosaicism is when an embryo has both normal and abnormal cells. It is often not transferred due to concerns about the potential risk of having a baby with a condition derived from this mosaicism. However, evidence is still emerging, and some suggest that there is overdiagnosis of mosaicism, leading to a reduction in cumulative live birth, which could impact those with fewer embryos.
Engaging in a Shared-Decision Process: How Patients and Physicians Should Approach PGT-A
It is important for patients and physicians to engage in a shared-decision making process when considering PGT-A. Patients should be informed about the current scientific discussion and uncertainty, while physicians should discuss with patients the known and unknown data to make informed decisions that consider patients’ values, preferences, and desires.

In conclusion, PGT-A has both benefits and drawbacks, and a deep discussion should occur to determine whether it is the right choice for each individual patient. As this is a topic that is actively being discussed in scientific meetings, patients should be aware of the latest findings and engage in a thorough discussion with their physicians.